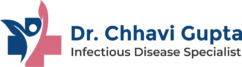
ATT-Induced Liver Dysfunction: A Serious Concern in TB Management
Understanding ATT and Its Role
Anti-tuberculosis therapy (ATT) is the standard treatment for tuberculosis, typically involving a combination of drugs like isoniazid, rifampicin, pyrazinamide, and ethambutol. While these drugs are effective, some of them carry a known risk of liver toxicity.
What Is ATT-Induced Liver Dysfunction?
ATT-induced liver dysfunction refers to liver damage that occurs as a side effect of TB medications. It often presents as elevated liver enzymes (transaminases), and in some cases, may progress to jaundice or even acute liver failure if left unmonitored.
Symptoms to Watch For
- Nausea and vomiting
- Abdominal pain (especially in the right upper quadrant)
- Jaundice (yellowing of eyes and skin)
- Fatigue or general weakness
- Dark-colored urine
Who Is at Risk?
Patients at higher risk for liver toxicity from ATT include:
- Those with pre-existing liver disease (e.g., hepatitis B or C)
- People with poor nutritional status
- Elderly individuals
- Those who consume alcohol regularly
- HIV-positive individuals
- Monitoring and Management
- Baseline Liver Function Tests (LFTs) should be done before starting ATT
- Routine monitoring is important, especially during the first two months
- If significant liver injury occurs, drugs may need to be paused and reintroduced gradually under expert guidance
- Modified regimens or hepatoprotective agents may be considered
Why Early Detection Matters
Delays in recognizing liver dysfunction can lead to serious complications and jeopardize TB treatment. Timely action can prevent permanent damage and allow patients to safely complete their course of therapy.
If you or someone you know is undergoing TB treatment and experiencing symptoms of liver dysfunction, consult an infectious disease specialist immediately.
Dr. Chhavi Gupta
MBBS, MD, DM (AIIMS, New Delhi)
Senior Consultant – Infectious Diseases
Yashoda Super Speciality Hospital, Kaushambi
📞 For Appointments: +91 8851 346 424
🌐 drchhavigupta.com