Do you Know Tuberculosis can cause infertility in females and males?
Dr. Chhavi Gupta
DM (Infectious disease), AIIMS, New Delhi
Senior Consultant, Yashoda Superpseciality Hospital, Kaushambi
The association between infection and infertility has been long known. The infections that manifest symptomatically are identified easily and timely and can be managed. However, infections that lead to asymptomatic infections or remain dormant are more damaging as lack of symptoms prevents a patient from seeking timely medical intervention and consequently chronic damage to reproductive organs.
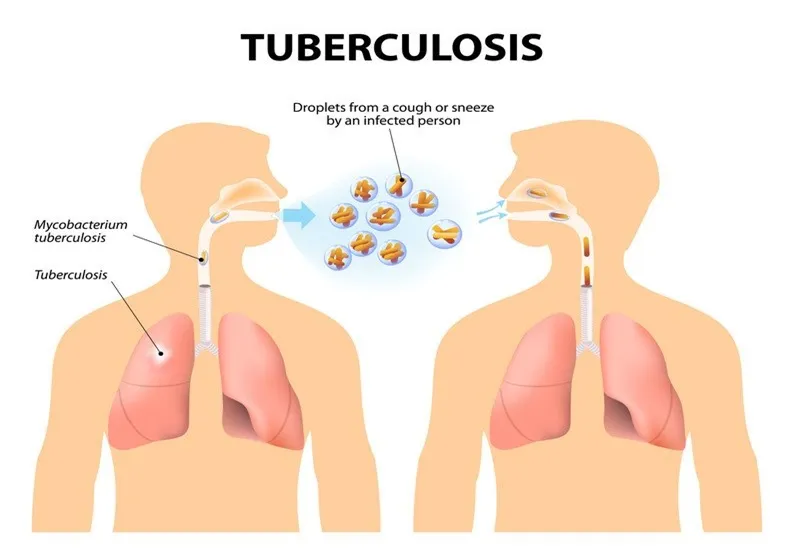
It is always believed by the common man that TB can affect only the lungs, but TB can affect any body part beyond the lung known as extrapulmonary TB (EPTB). TB affecting reproductive organs, also known as Genitourinary TB is responsible for 27.1 per cent cases of EPTB. The exact incidence of female genitourinary TB is not known because of vague symptomatology or asymptomatic cases, lack of sensitive diagnostic tests, and cases are not underreported. Genital TB mostly spreads from the lungs or other organs via blood or sometimes directly spreads from adjacent organs like abdominal TB or may be sexually transmitted from active genitourinary TB in the partner.
Female Genitourinary TB and Infertility
TB causes both functional and physiological damage to the reproductive system. Genital TB in females affect most commonly fallopian tubes (90% of cases) leading to tubal blockage, and the uterus in 70% of cases resulting in decreased endometrial receptivity for implantation of a fertilized egg; ovaries are affected in 20-25 % of cases resulting in poor egg formation. Apart from affecting organs, Genital Tb also causes disturbance in the immune system, which may interfere with the implantation of fertilized eggs in the uterus. Thus, genital TB in females not only affect conception but also the ability to carry pregnancy. Further, it is important to note that not only genital TB causes infertility but TB affecting any other organ in the body causes malnutrition, immune disturbances, and impaired hormone production which can lead to poor egg formation or secondary amenorrhoea resulting in infertility.
Infertility treatment and risk of TB
As we learned TB is one of the main reasons for infertility but vice versa is there. Reactivation of TB can occur after surgical manipulation, high steroid levels, immune system perturbations, and increased vascularity during ovarian stimulation are thought to be the triggering factors for TB reactivation.
Male Genitourinary TB and Infertility
Genital TB in males predominantly causes structural damage to the male reproductive system. About 10% of patients with male genital TB may present with infertility, and around 4.0–9.1% of such men may have poor semen quality. Sometimes, scarring and fibrosis may persist even after successful treatment of TB. Similar to females, males may also remain asymptomatic or they may present as an unexplained, gradually progressing decline in semen quality or sometimes TB is picked incidentally during diagnostic workup. Sometimes, TB of any other part of the body apart from genital TB can affect the overall health of males leading to malnutrition and oligospermia.
Genital TB is a paucibacillary disease, i.e. number of tuberculosis bacteria that can be detected is very scanty, hence the diagnosis is very difficult. The diagnostic work requires complete investigations like blood test, radiology test, endometrial biopsies or aspirate followed by pathological or microbiological conformation. Sometimes in absence of appropriate diagnostic test, patients end up in taking tuberculosis treatment based on suspicious or misleading diagnostic test, this may be equally harmful as unnecessary tuberculosis treatment may promote drug resistant tuberculosis.
Genital TB is a complex and chronic infection that can affect reproductive system of both males or females resulting in infertility. Early detection and treatment can prevent irreversible damage but being paucibacillary disease, diagnosis remains difficult. With recent advancement in diagnostic test, detailed history and meticulous examination and diagnostic work up is key to success. Couple must seek specialist opinion before starting tuberculosis treatment for infertility.