IBD vs Intestinal Tuberculosis: The Role of the Infectious Disease Specialist
Intestinal Tuberculosis (TB) and Inflammatory Bowel Disease (IBD) are two conditions that can appear strikingly similar in clinical presentations, making diagnosis a challenging process. Differentiating between these two is crucial, as their treatments are entirely different—and a wrong diagnosis can lead to harmful outcomes.
Similar Symptoms, Different Causes
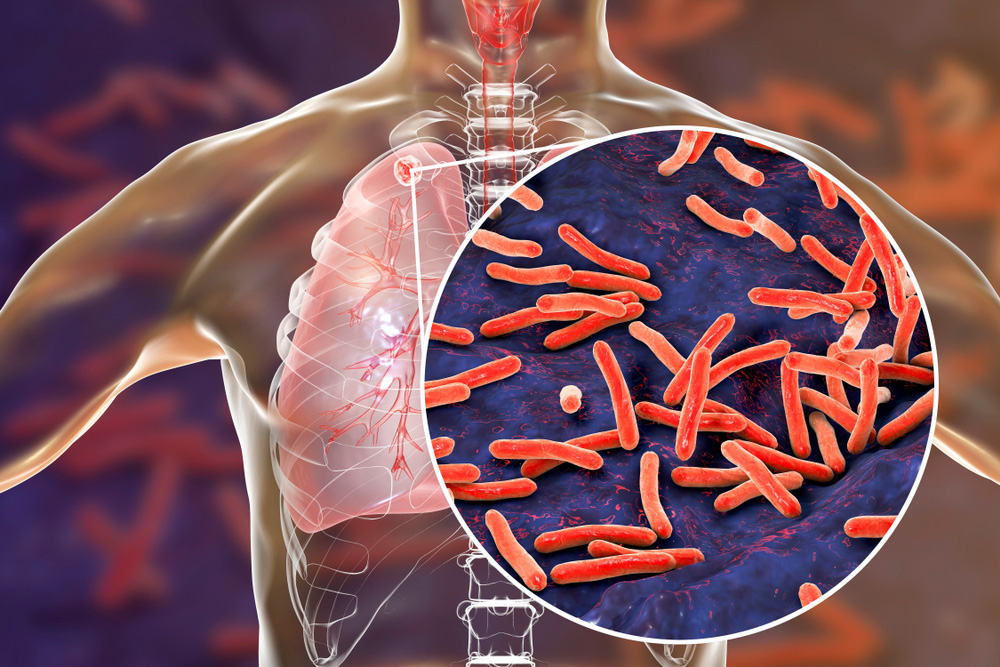
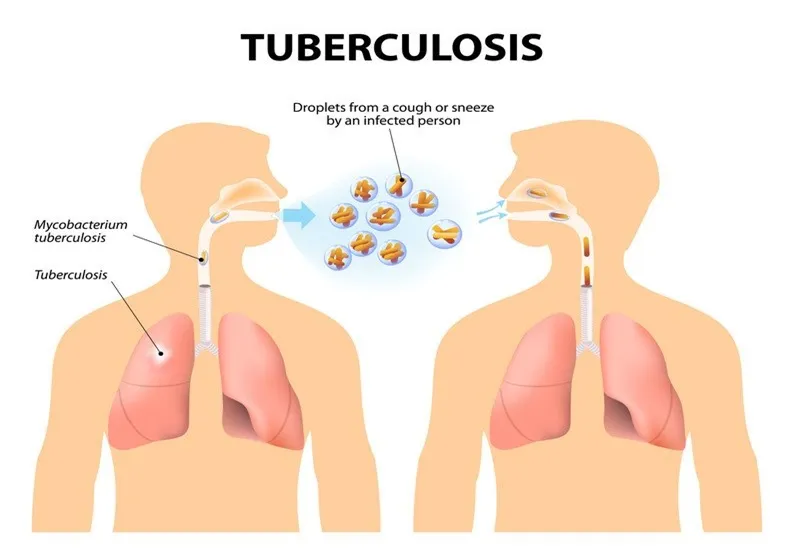
IBD, which includes Crohn’s disease and ulcerative colitis, is an autoimmune condition where the body attacks its own gut lining. Intestinal TB, on the other hand, is a bacterial infection caused by Mycobacterium tuberculosis affecting the gastrointestinal tract.
Common symptoms of both include:
- Chronic abdominal pain
- Diarrhea or altered bowel habits
- Weight loss
- Low-grade fever
- GI bleeding
Despite these similarities, the underlying pathology is very different, which is why the expertise of an Infectious Disease (ID) Specialist is essential.
Why Infectious Disease Evaluation is Key
An ID specialist is trained to detect signs of chronic infections like TB that may mimic autoimmune diseases. They conduct targeted investigations including:
- PCR testing or GeneXpert for TB DNA
- Histopathology from biopsies
- Mantoux (Tuberculin) tests and IGRA (Interferon Gamma Release Assays)
- Radiological imaging (e.g., CT, MRI)
A thorough infectious workup can prevent the dangerous consequence of misdiagnosing intestinal TB as IBD and wrongly starting immunosuppressants, which can allow TB to disseminate.
- Treatment: A Delicate Balance
- Intestinal TB is treated with a full course of Anti-Tubercular Therapy (ATT) for 6–9 months.
IBD often requires long-term immunosuppression (steroids, biologics, etc.).
Starting immunosuppressive treatment in a patient with undiagnosed TB can be fatal. Hence, ruling out TB thoroughly before initiating IBD treatment is a standard recommendation, especially in endemic countries like India.
Clinical Clues That Favor TB Over IBD:
- History of TB exposure or past TB
- Presence of lung lesions on chest X-ray
- Shorter duration of illness
- Involvement of the ileocecal region
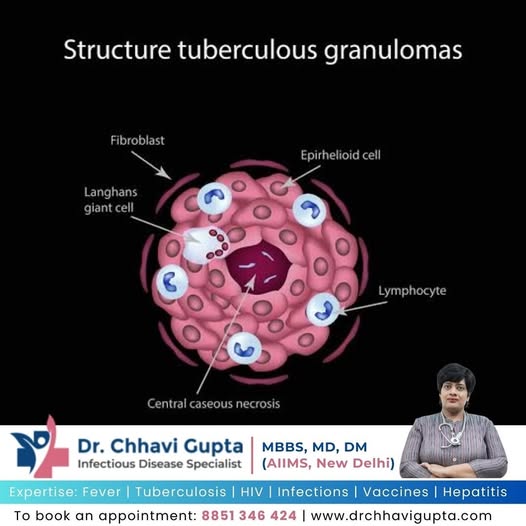
- Presence of caseating granulomas on biopsy
When to Consult an Infectious Disease Specialist
- When dealing with unexplained chronic GI symptoms
- When biopsy shows granulomas or features that are not classic for IBD
- Before starting immunosuppressive treatment in suspected IBD
- If there is a lack of response to standard IBD therapies
Remember: Not all granulomatous colitis is IBD—some are TB.
Consult an infectious disease expert to avoid misdiagnosis and ensure safe, effective treatment.
👩⚕️ Dr. Chhavi GuptaMBBS, MD, DM (AIIMS, New Delhi)Senior Consultant – Infectious Diseases📍 Yashoda Super Speciality Hospital, Kaushambi📞 For Appointments: +91 8851 346 424🌐 drchhavigupta.com